Climate Change and Health
The Intergovernmental Panel on Climate Change (IPCC) released its latest report on March 31, 2014. This report was the second instalment of the Fifth Assessment Report, prepared by Working Group 2, on impacts, vulnerability, and adaptation to climate change [1]. In this Comment, we, as contributors to the chapter on human health, explain how the IPCC report was prepared and highlight important findings.
The IPCC reviews and assesses the scientific published work on climate change. As an intergovernmental body composed of members of the UN, the IPCC does not undertake research itself; instead it appoints Working Groups who assess the work. This assessment means more than simply to summarise the state of knowledge: Working Groups are asked to weigh what has been written (in both peer-reviewed publications and grey literature), to make judgments about likelihood and uncertainty, and to flag important emerging issues [2]. The focus for Working Group 2 was mainly, but not exclusively, on what had been written since the previous assessment in 2007 [3]; papers were eligible for inclusion if they were published, or accepted for publication, before Aug 31, 2013. The Working Groups were required to highlight what might be relevant to policy, but did not recommend policies. The Fifth Assessment Report Working Group 1 reported on the physical science of climate change [4] in September, 2013 (appendix). Working Group 3, concerned with mitigation (ie, reduction of greenhouse gas emissions), will release its report in April, 2014.
The scale of the enterprise is remarkable—indeed, reports by the IPCC together probably represent the largest scientific assessment exercise in history. There are 310 authors and review editors in Working Group 2, and an even greater number of contributing authors who have added to the report from their areas of special expertise. In addition to health, Working Group 2 examined natural and managed resources (eg, fresh water, coastal systems, and food production), human settlements, and other aspects of wellbeing such as security and livelihoods. The report (30 chapters) will be published in two volumes, and includes integrated assessments of impacts and adaptation in nine geographic regions and an overarching summary for policy makers.
Work on the Fifth Assessment Report began 5 years ago (appendix) and aspects of the IPCC process distinguish its assessments from other reviews and scientific publications. One difference is the substantial role of member states in determination of, in the initial stages, the scope of the reports and the membership of writing groups. At the beginning of each round of assessment, meetings organised by the IPCC decide on the structure of the reports, including the number of chapters and the topics to be covered, and then member states nominate potential authors. The final decision about authors is made by a subgroup from the IPCC, the Bureau, on the basis of scientific merit and the necessary institutional and disciplinary perspectives for each chapter, seeking, at the same time, to achieve a balance of representation by gender and region. Once appointed, the IPCC authors work independently; government input occurs as part of the peer review process. However, the member states must approve and sign off on the final report. Thus, the IPCC assessments are the outputs of many iterative interactions between scientists and policy makers.
Another feature of the IPCC process is the intensity of peer review. There were four rounds of review for the Fifth Assessment Report, two of which involved hundreds of self-nominated experts and scientists appointed by member-state governments. Each round generated an enormous number of comments, questions, and requests for change. For instance, the IPCC received 1009 reviewer comments just on the second-order draft of chapter 11 (human health). Two dedicated review editors per chapter are charged with ensuring that the authors consider each comment seriously and, if they reject it, that they do so with good reasons. Both the comments and the chapter authors’ responses will be published on the IPCC website.
The IPCC does not prescribe how chapter groups should gather and interpret the scientific work, partly because conventions and practice differ among disciplines. Contributors to the health chapter used many strategies to identify relevant published work. Due to the breadth of the topic, including the range of health outcomes and exposure pathways, the chapter team decided that one systematic review would not be possible.
Executive summary, chapter 11. Human health: impacts, adaptation and co-benefits. From the Report of Working Group 2, Intergovernmental Panel on Climate Change, Fifth Assessment Report [1]
“The health of human populations is sensitive to shifts in weather patterns and other aspects of climate change [very high confidence]. These effects occur directly, due to changes in temperature and precipitation and occurrence of heat waves, floods, droughts, and fires. Indirectly, health may be damaged by ecological disruptions brought on by climate change (crop failures, shifting patterns of disease vectors), or social responses to climate change (such as displacement of populations following prolonged drought). Variability in temperatures is a risk factor in its own right, over and above the influence of average temperatures on heat-related deaths. Biological and social adaptation is more difficult in a highly variable climate than one that is more stable.
Until mid-century, climate change will act mainly by exacerbating health problems that already exist [very high confidence]. New conditions may emerge under climate change [low confidence], and existing diseases (e.g. food-borne infections) may extend their range into areas that are presently unaffected [high confidence]. But the largest risks will apply in populations that are currently most affected by climate-related diseases. Thus, for example, it is expected that health losses due to climate change-induced under-nutrition will occur mainly in areas that are already food-insecure.
In recent decades, climate change has contributed to levels of ill-health [likely] though the present world-wide burden of ill-health from climate change is relatively small compared with other stressors on health and is not well quantified. Rising temperatures have increased the risk of heat-related death and illness [likely]. Local changes in temperature and rainfall have altered distribution of some water-borne illnesses and disease vectors, and reduced food production for some vulnerable populations [medium confidence].
If climate change continues as projected across the [Representative Concentration Pathways] scenarios, the major increases of ill-health compared to no climate change will occur through:
- Greater risk of injury, disease, and death due to more intense heat waves and fires [very high confidence];
- Increased risk of under-nutrition resulting from diminished food production in poor regions [high confidence];
- Consequences for health of lost work capacity and reduced labor productivity in vulnerable populations [high confidence];
- Increased risks of food- and water-borne diseases [very high confidence] and vector-borne diseases [medium confidence];
- Modest reductions in cold-related mortality and morbidity in some areas due to fewer cold extremes [low confidence], geographical shifts in food production, and reduced capacity of disease-carrying vectors due to exceedance of thermal thresholds [medium confidence]. These positive effects will be increasingly out-weighed, world-wide, by the magnitude and severity of the negative effects of climate change [high confidence].
Impacts on health will be reduced, but not eliminated, in populations that benefit from rapid social and economic development [high confidence], particularly among the poorest and least healthy groups [very high confidence]. Climate change is an impediment to continued health improvements in many parts of the world. If economic growth does not benefit the poor, the health effects of climate change will be exacerbated.
In addition to their implications for climate change, essentially all the important Climate Altering Pollutants (CAPs) other than CO2 have near-term health implications [very high confidence]. In 2010, more than 7% of the global burden of disease was due to inhalation of these air pollutants [high confidence].
Some parts of the world already exceed the international standard for safe work activity during the hottest months of the year. The capacity of the human body to thermoregulate may be exceeded on a regular basis, particularly during manual labour, in parts of the world during this century. In the highest Representative Concentration Pathway, RCP8.5, by 2100 some of the world’s land area will be experiencing 4–7 degree higher temperatures due to anthropogenic climate change [WG1, Figure SPM.7]. If this occurs, the combination of high temperatures and high humidity will compromise normal human activities, including growing food and other work outdoors, in some areas, for parts of the year [high confidence].
The most effective measures to reduce vulnerability in the near-term are programs that implement basic public health measures such as provision of clean water and sanitation, secure essential health care including vaccination and child health services, increase capacity for disaster preparedness and response, and alleviate poverty [very high confidence]. In addition, there has been progress since [Fourth Assessment Report] in targeted and climate-specific measures to protect health, including enhanced surveillance and early warning systems.
There are opportunities to achieve co-benefits from actions that reduce emissions of CAPs and at the same time improve health. Among others, these include:
- Reducing local emissions of health-damaging and climate-altering air pollutants from energy systems, through improved energy efficiency, and a shift to cleaner energy sources [very high confidence].
- Providing universal access to reproductive health services (including modern family planning) to improve child and maternal health through birth spacing and reduce population growth, energy use, and consequent CAP emissions over time [medium confidence];
- Shifting consumption away from animal products, especially from ruminant sources, in high-meat-consumption societies toward less CAP-intensive healthy diets [medium confidence].
- Designing transport systems that promote active travel and reduce use of motorized vehicles, leading to lower emissions of CAPs and better health through improved air quality and greater physical activity [high confidence].
There are important research gaps regarding the health consequences of climate change and co-benefits actions, particularly in low-income countries. There are now opportunities to use existing longitudinal data on population health to investigate how climate change affects the most vulnerable populations. Another gap concerns the scientific evaluation of the health implications of adaptation measures at community and national levels. A further challenge is to improve understanding of the extent to which taking health co-benefits into account can offset the costs of [greenhouse gases] mitigation strategies.
They followed a published search protocol [5] to identify relevant articles and used other approaches to ensure that there were no important omissions, including cross-checks with other reviews. In selection of references for the chapter, contributors gave priority to publications that were recent, added important new findings to the literature, included areas or population groups that had not previously been well described, or were judged to be particularly relevant to policy in other respects.
The IPCC uses two means to communicate certainty related to findings. One is a confidence statement, a qualitative assessment “based on the type, amount, quality, and consistency of evidence (eg, mechanistic understanding, theory, data, models, expert judgment, etc) and the degree of agreement” [6]. This confidence ranges from very low (as might arise when there is limited evidence and little agreement between researchers) to very high (typically needs robust evidence and high agreement). Authors can also apply a likelihood statement, which aims to provide “calibrated language for described quantified uncertainty” [6]. On this scale, virtually certain means 99–100% probability, with diminished likelihood for very likely (90–100%), likely (66–100%), about as likely as not (33–66%), unlikely (0–33%), and very unlikely (0–10%).
The major findings of the health chapter in the Fifth Assessment Report are included in the executive summary (panel) and in the figure.1 Many conclusions echo those of the Fourth Assessment Report [3]. For instance, once again, the report projects that climate change will act mainly, at least in the medium term (to the middle of this century), through exacerbation of health problems that already exist, and the largest risks are to populations whose health and wellbeing are most affected by the present- day climate. The Fourth Assessment Report listed the following as the main pathways by which climate change might affect health—undernutrition from reductions in food production, injury and disease due to intense heatwaves and fires, and shifts in the timing and spatial distribution of infectious diseases [3]. According to the Fifth Report, these factors remain important.
What is new in the Fifth Report? The health outcomes and other consequences of lost work capacity and reduced labour productivity due to rising temperatures are not new subjects, but they receive much more attention in this report than they did previously because the scientific published work has grown considerably. The Fifth Report also gives greater attention to the so-called high-end climate scenarios, reflecting recent research and the persistent failure of international negotiations to make credible progress toward substantial reduction in emissions. Some scenarios project warming of 4–7°C (on average) over much of the global landmass by the end of the 21st century [7]. If this change happens, then the hottest days will exceed present temperatures by a wide margin and increase the number of people who live in conditions that are so extreme that the ability of the human body to maintain heat balance during physical activity is compromised for parts of the year and unprotected outdoor labour is no longer possible. Other risks are associated with high-end scenarios, for instance, those affecting urban settlements, food production, and water resources. These were described elsewhere in the report of Working Group 2.
The new assessment concluded, as did the Fourth Report, that there might be some health gains from climate change (such as reduced cold-related morbidity and mortality), but showed that the evidence is now stronger for positive effects to be outweighed, worldwide, by negative effects. The effect of climate-sensitive health outcomes (such as hunger and vector-borne diseases) is moderated by many factors other than climate (eg, living conditions and health care). The Fifth Assessment Report drew on studies that modelled, for the first time, the potential health consequences of changes in climate alongside projected social and economic changes. This research shows how climate change opposes health gains achieved by social development and that it might hold back progress in the poorest countries.
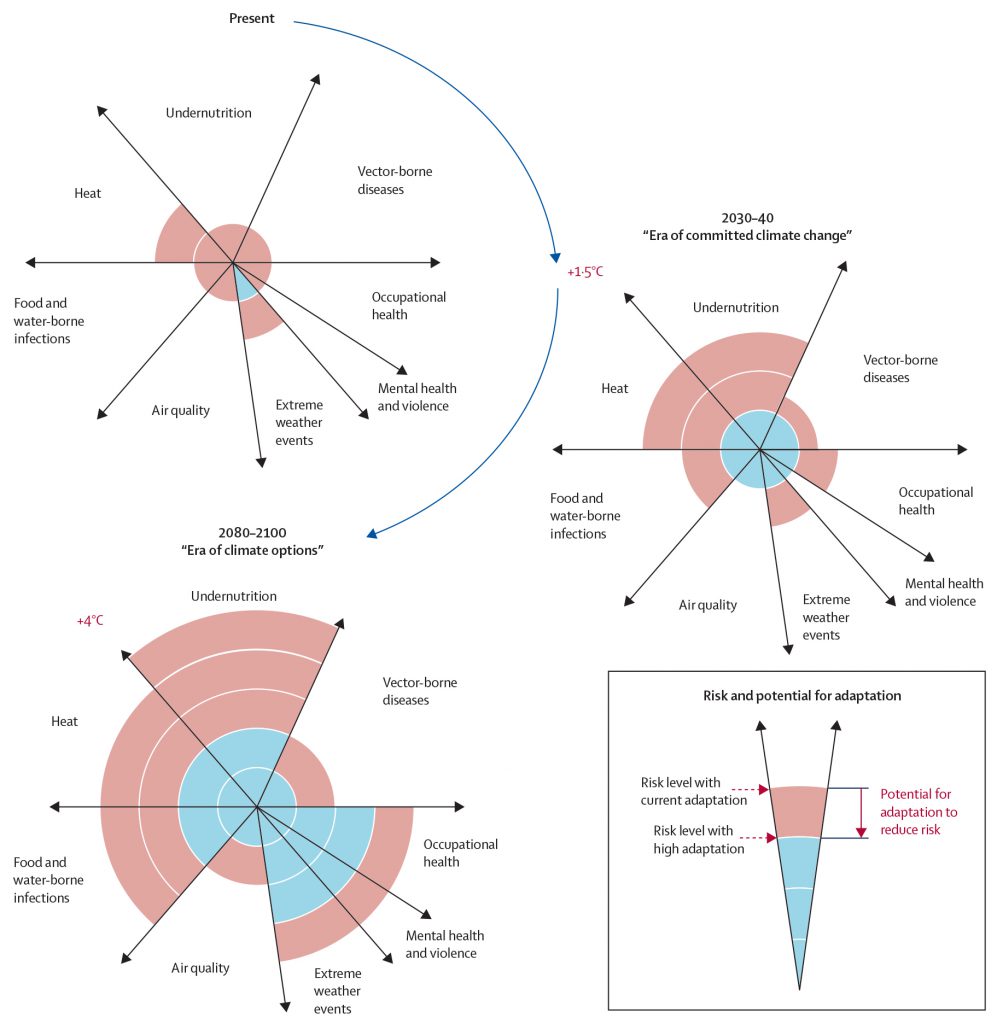
Figure: Conceptual presentation of the health outcomes from climate change and the potential for reduction through adaptation Outcomes were identified in eight health-related sectors on the basis of assessment of the published work and expert judgments by the authors. The width of the slices qualitatively indicates the relative burden caused to ill-health worldwide at present and should not be considered completely independent. Effect levels are presented for the near-term era of committed climate change (2030–40), in which projected levels of global mean temperature increases do not diverge substantially across emissions scenarios. For some sectors—eg, vector-borne diseases, hot or cold stress, and agricultural production and undernutrition—there might be benefits to health in some areas, but net effect is expected to be negative. Although occupational health outcomes are probably largely related to thermal stress, they exist separately from heat effects in the figure because mainly they affect different groups within the population. Estimated effects are also presented for the longer-term era of climate options (2080–2100), for global mean temperature increase of about 4°C higher than preindustrial levels, which could potentially be avoided by vigorous mitigation efforts done soon. For each timeframe, effect levels are estimated for the current state of adaptation and for a hypothetical highly adapted state, indicated by different colours. Based on Figure 11.6 in the report of Working Group 2, chapter 11.1
The most effective adaptation measures for health in the near-term are programmes that implement or improve basic public health measures where needed. However, further climate-specific measures (such as early warning systems for extreme weather) will be needed to protect the health of a population, even in high-income countries, as climate change proceeds. This need has been shown by extreme events such as the heatwaves and fires in Australia in 2009 and Russia in 2010 [8], [9].
We note that the full title of chapter 11 is “Human health: impacts, adaptation and co-benefits”. Co- benefits (which were not discussed separately in the Fourth Assessment Report) are defined in the chapter as “health gains from strategies that are directed primarily at climate change and mitigation of climate change from well-chosen policies for health advancement”. Examples include reduction of health-damaging emissions from both large-scale energy systems (power stations) and local energy sources (eg, biomass and coal stoves); transport improvements that favour public transport, walking, and cycling, instead of private motor vehicles; provision of access to reproductive health services for individuals who wish to restrict family size (leading to health gains, particularly in low-income countries, and long-term reductions in emissions); and the promotion of healthy, low-greenhouse-gas-emission diets, including reduced consumption of animal products. The health co-benefits of action on climate change could be very large. For instance, a reduction of emissions of methane and black carbon might directly prevent 2·0–2·5 million deaths per year worldwide, according to one estimate [10]. When converted into economic terms, the health gains could offset much of the early cost for mitigation of climate change. The purpose of the IPCC assessment is to assist policy makers as they wrestle with the long- term, large-scale challenges of climate change. We hope that the information contained in the Fifth Assessment Report will provide both motivation and means to hasten meaningful, effective climate agreements.
Alistair Woodward, Kirk R Smith, Diarmid Campbell-Lendrum, Dave D Chadee, Yasushi Honda, Qiyong Liu, Jane Olwoch, Boris Revich, Rainer Sauerborn, Zoë Chafe, Ulisses Confalonieri, Andy Haines
School of Population Health, University of Auckland, Auckland 1142, New Zealand (AW); School of Public Health, University of California, Berkeley, CA, USA (KRS, ZC); Department of Public Health, Environmental and Social Determinants of Health, WHO, Geneva, Switzerland (DC-L); Department of Life Sciences, University of West Indies, St Augustine, Trinidad and Tobago (DDC); Faculty of Health and Sports Sciences, University of Tsukuba, Tsukuba, Japan (YH); State Key Laboratory for Infectious Disease Prevention and Control, National Institute for Communicable Disease Control and Prevention, China Center for Disease Control and Prevention, Beijing, China (QL); SANSA Earth Observation, South African National Space Agency, Pretoria, South Africa (JO); Institute of Forecasting, Russian Academy of Science, Moscow, Russia (BR); Department of Public Health and Clinical Medicine, Umeå University, Umeå, Sweden (RS); Laboratory of Health Education, FIOCRUZ Oswaldo Cruz Foundation, Belo Horizonte, Brazil (UC); and Department of Social and Environmental Health Research, London School of Hygiene & Tropical Medicine, London, UK (AH) a.woodward@auckland.ac.nz
KRS and AW were coordinating lead authors of chapter 11 of the Fifth Assessment Report of the IPCC; DC-L, DDC, YH, BR, JO, QL, and RS were lead authors; ZC was chapter scientist; and AH and UC were review editors. We acknowledge the following contributing authors for chapter 11: Clara Aranda, Helen Berry, Colin Butler, Zoë Chafe, Lara Cushing, Kris Ebi, Tord Kjellstrom, Sari Kovats, Graeme Lindsay, Erin Lipp, Tony McMichael, Virginia Murray, Osman Sankoh, Marie O’Neill, Seth Shonkoff, Joan Sutherland, and Shelby Yamamoto. Joacim Rocklov was chapter scientist 2010–11. We thank Andy Reisinger for his helpful comments on an earlier version of this Comment. We declare that we have no competing interests.
References
- Field CB, Barros V, Dokken DJ, et al. Climate change 2014: impacts, adaptation, and vulnerability. Volume I: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge and New York: Cambridge University Press, 2014.
- Ebi KL. Key themes in the Working Group II contribution to the Intergovernmental Panel on Climate Change 5th Assessment Report. Climatic Change 2012; 114: 417–26.
- Parry ML, Canziani OF, Palutikof JP, van der Linden PJ, Hanson CE. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change, 2007. Cambridge: Cambridge University Press, 2007.
- Stocker TF, Qin D, Plattner G-K, et al. Climate change 2013: the physical science basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge and New York: Cambridge University Press, 2013.
- Hosking J, Campbell-Lendrum D. How well does climate change and human health research match the demands of policymakers? A scoping review. Environ Health Perspect 2012; 120: 1076–82.
- Mastrandrea MD, Mach KJ, Plattner G-K, et al. The IPCC AR5 guidance note on consistent treatment of uncertainties: a common approach across the working groups. Climatic Change 2011; 108: 675–91.
- The World Bank. Turn down the heat. Why a 4°C warmer world must be avoided. A report for the World Bank by the Potsdam Institute for Climate Impact Research. Washington, DC: The World Bank, 2012.
- Teague B, McLeod R, Pascoe S. 2009 Victorian Bushfires Royal Commission final report. Melbourne: Parliament of Victoria, 2010. http:// www.royalcommission.vic.gov.au/Commission-Reports/Final-Report (accessed March 28, 2014).
- Shaposhnikov D, Revich B, Bellander T, et al. Mortality related to interactions between heat wave and wildfire air pollution during the summer of 2010 in Moscow. Epidemiology 2014; published online March 4. DOI:10.1097/EDE.0000000000000090.
- Anenberg SC, Schwartz J, Shindell D, et al. Global air quality and health co-benefits of mitigating near-term climate change through methane and black carbon emission controls. Environ Health Perspect 2012; 120: 831–39.
© 2014. World Health Organization. Published by Elsevier Ltd/Inc/BV. All rights reserved.